Talking About In‑Home Care with Family During the Holidays: Practical Tips and Next Steps
Holiday visits often surface changes in a loved one’s daily abilities — and that makes these gatherings a natural time to raise the topic of in‑home care. When relatives spend concentrated time together, it’s easier to notice mobility, medication routines, and social engagement that might look different than during a short phone call. This guide walks you through spotting concerns, starting compassionate conversations, organizing family decision‑making, and taking concrete next steps like scheduling an assessment. You’ll find practical conversation tips, sample scripts for talking with aging parents, an easy checklist of signs a senior may need help at home, and strategies to ease caregiver stress during the holidays. The sections that follow explain what to observe, how to document objective incidents, ways to open sensitive talks without causing defensiveness, and how to include siblings and other family members in a clear plan. Finally, we outline in‑home assessment basics, common service types (personal care, companion care, medication support), and short‑term respite options to protect caregiver well‑being.
Why the Holidays Are a Good Time to Talk About In‑Home Care
Holidays bring more people, more activity, and longer visits — a combination that often highlights changes in mobility, cognition, and daily routines. The contrast between usual life and holiday rhythms — travel, extended family time, and large meals — can reveal fatigue, confusion, or missed medications that might not show up in a quick weekday check‑in. Raising concerns while observations are fresh helps frame the conversation as a practical step for safety and comfort, not as an abrupt loss of independence. Below we’ll cover what to watch for during gatherings and tactics for managing emotional and practical barriers to productive talks.
How Holiday Gatherings Reveal Care Needs
Holidays naturally create many moments to observe everyday functioning: standing up from the dinner table, walking to another room, getting a coat, or managing a plate at the buffet. Family members can note specific, objective incidents — for example, hesitating when standing, looking confused at the door, or missing doses when medicines are visible — and record dates and context for later discussion.
Keep observations focused on actions and episodes rather than labels or judgments. Designating one person to take short, factual notes during the visit helps turn anecdotes into usable evidence for follow‑up conversations and assessment planning.
Common Challenges When Discussing Care at the Holidays
Denial, guilt, and heightened emotions often complicate practical decisions about care. Seniors may fear losing independence; relatives can disagree about urgency, costs, or who will manage tasks; and holiday stress can intensify reactions. To reduce conflict, plan a private follow‑up conversation after the visit, use neutral language, and avoid surprising your loved one. These steps set the stage for a structured checklist and a clear assessment that connects observations to realistic care options.
Research shows that deeply held ideas about filial duty can add complexity to holiday care conversations and family dynamics.
Filial Duty & Holiday Care Conversations This study examines how expectations of filial duty during holidays shape intergenerational relationships and caregiving roles, based on the experiences of Norwegian midlife single women. Holidays with aging parents: Pleasures, duties and constraints, B Heimtun, 2019
Key Signs a Loved One May Need In‑Home Care
Signs that a senior might benefit from in‑home support cover physical, cognitive, environmental, and social areas — and they become most useful when clearly documented during visits. Watch for changes in mobility, hygiene, medication management, thinking, and household upkeep to build a prioritized list of red flags to discuss with clinicians or care assessors. Using an objective checklist with a simple threshold (for example, three or more red flags) gives families a clear prompt to pursue a professional evaluation. Below is a practical checklist and a table that turns observations into actionable notes you can compare across visits.
The following list highlights scannable indicators to watch for during holiday visits:
Frequent falls or near‑falls: Repeated balance problems or an unsteady gait at home.
Medication mismanagement: Missed doses, double dosing, or confusion about prescriptions.
Decline in personal hygiene: Noticeable changes in grooming, bathing, or clean clothing.
Cognitive changes: More forgetfulness, disorientation, or trouble following conversations.
Household neglect: Unsafe conditions, spoiled food, or unmanaged bills and piling mail.
Social withdrawal or mood changes: Loss of interest in activities, increasing sadness, or irritability.
If several of these items are present, consider a professional evaluation — three or more red flags commonly indicate the need for a formal in‑home care assessment to identify appropriate supports.
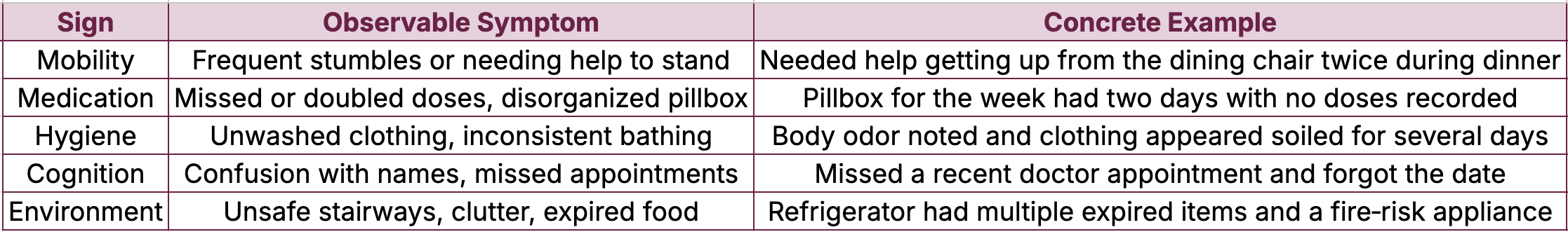
Signs table intro: The table below converts common signs into observable symptoms and concrete examples to help families record incidents clearly during holiday visits.
This table helps families turn observations into objective documentation that supports a clear conversation and, if necessary, a referral for a formal assessment.
Which Physical and Cognitive Indicators Signal the Need for Help?
Physical and cognitive red flags include repeated falls, difficulty with ADLs (activities of daily living) like dressing or toileting, and memory lapses that interfere with daily decisions. Note how often incidents happen and the context — for example, whether balance issues occur only during unfamiliar tasks or during routine activities. Cognitive signs such as repeatedly missed appointments, medication mistakes, or getting lost in a familiar area suggest the need for supervision or medication support. Objective, dated examples strengthen the case for follow‑up assessment and help evaluators match services (personal care, medication management) to the senior’s needs.
Using a Comprehensive Checklist to Identify Needs
A thorough checklist scores observations across ADLs, IADLs, medication, home safety, and emotional well‑being. Families can use a simple threshold (for example, three or more red flags) to trigger an assessment. Good documentation includes dates, who witnessed the incident, and a brief description to separate facts from feelings. Typical next steps after scoring include a private family conversation, scheduling a complimentary in‑home care assessment, and putting short‑term supports in place (companion care or respite) while longer‑term options are considered. Clear thresholds and organized notes keep the focus on safety and quality of life, reducing conflict.
How to Start In‑Home Care Conversations with Empathy and Clarity
Begin care conversations from shared values: express concern, cite specific observations, and present options rather than ultimatums. Ask permission before sharing what you noticed, then read a short, objective incident log from the holiday visit. Offer a menu of next steps — from a short respite trial to regular companion visits — and suggest a concrete next action like a professional assessment to clarify needs. Below you’ll find sample scripts, timing advice, and approaches for responding to resistance while protecting dignity.
Person‑centered communication is key: focusing on the older person’s needs and preferences improves the experience and outcomes of in‑home care discussions.
Person‑Centered Communication in Home Care This research highlights communication challenges in home care and argues for person‑centered policies and guidelines that support better interactions between care professionals and older adults. Communicative challenges in the home care of older persons – a qualitative exploration, AJ Sundler, 2016
The numbered list below gives a clear, step‑by‑step approach to opening a care conversation:
Open with empathy and ask permission: Start by asking if you can share something you noticed and make your concern clear.
Stick to specific observations, not labels: Use dates and incidents instead of generalities.
Offer practical options and support: Present short‑term steps and emphasize teamwork.
Recommend a neutral assessment: Suggest a professional evaluation to turn observations into a plan.
Best Strategies for Talking with Aging Parents
Keep openings short, non‑accusatory, and rooted in specific observations. For example: “I noticed you were very tired after dinner and needed help standing twice — can we talk about making evenings easier for you?” Choose a calm, private moment away from the main holiday activity to avoid overwhelm. If conversations tend to escalate, consider inviting a neutral third party (a physician, pastor, or social worker) to join. End the initial talk with a clear next step, such as scheduling a free in‑home care assessment — this moves the discussion from opinion to an evidence‑based plan.
Professional support can translate family observations into practical recommendations. Many in‑home senior care providers offer complimentary needs assessments to tailor suggestions. A brief evaluation can confirm whether options like personal care, companion care, medication management, or skilled nursing are appropriate and can ease family tension by offering an impartial perspective. Scheduling a free in‑home care assessment helps map checklist findings to a customized care plan that balances safety and independence while outlining next steps and trial services.
Handling Resistance and Denial
Resistance usually comes from fear of losing control, dependence, or embarrassment. Respond by validating feelings, repeating objective observations, and proposing reversible, low‑commitment steps. Try a phrase like: “I know this sounds like a big change. I’m worried about your safety after seeing you trip twice — could we try daily companion visits for a short trial?” Offer a time‑limited plan and schedule a follow‑up check‑in to reduce the sense of permanence. If progress stalls, suggest an independent medical evaluation or a free in‑home care assessment to bring professional input without emotional pressure.
How to Include All Family Members in Care Planning
Inclusive planning needs a clear agenda, assigned roles, and neutral facilitation so family dynamics don’t derail decisions. Set a meeting with objective notes, designate a decision lead for logistics, a financial lead for budgeting and insurance, and a medical liaison to gather clinical information. Document decisions, set revisit dates, and assign tasks to foster accountability. The list below outlines practical roles and a simple meeting structure to guide coordination.
Understanding family decision‑making dynamics — and how formal and informal care interact — helps create workable plans.
Family Decision‑Making for Formal and Informal Care This work models how family members together choose levels of informal and formal care for noninstitutionalized elderly relatives as part of a broader decision process. Formal home health care, informal care, and family decision making, D Byrne, 2009
Decision Lead: Schedules meetings and handles logistics.
Financial Lead: Gathers insurance details, budgets, and payment options.
Medical Liaison: Collects medical records, medication lists, and clinician input.
Care Coordinator: Manages daily scheduling and communication with caregivers.
Managing Family Dynamics to Reach Consensus
Use a meeting agenda, neutral facilitation, and clear decision rules (for example, majority with documented minority opinions). Start by stating shared goals — safety, independence, dignity — then review objective observations and checklist findings to agree on facts before discussing preferences. Record a written plan with assigned tasks and timelines, and set a trial period for any services with a follow‑up meeting to evaluate results. If conflicts persist, bring in a mediator or professional assessor for impartial recommendations tied to documented needs.
How Siblings Can Work Together During the Holidays
Siblings can divide responsibilities to maximize observation and reduce duplication: one person handles errands, another focuses on documenting observations, and a third provides emotional support and companionship. Use a short shared message to summarize observations, actions taken, and next steps to keep communication clear without emotional spillover. Agree ahead of time who will arrange follow‑up tasks — for example, scheduling a free in‑home care assessment or setting up respite if the checklist threshold is met. Coordinated, documented follow‑through after the holiday visit preserves continuity of care and lowers burnout risk.
Benefits and Process of an In‑Home Care Needs Assessment
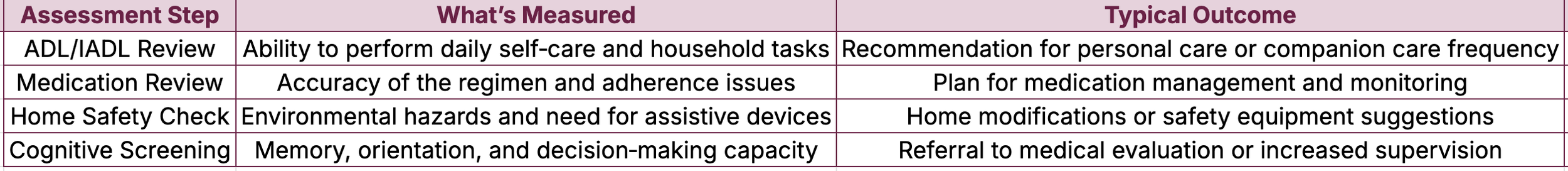
A professional in‑home care assessment reviews ADLs and IADLs, checks medications, evaluates home safety, and clarifies care goals to create a tailored plan that preserves independence while reducing risk. Assessors observe mobility, cognition, medication routines, and the living environment to recommend services — from companion care to personal care or skilled nursing — and to estimate frequency and intensity of support. Benefits include an impartial expert view, a documented care plan for family consensus, and actionable next steps such as trial visits or respite scheduling. The table below outlines typical assessment steps, what they measure, and the usual outcomes so families know what to expect from a complimentary in‑home assessment.
Assessment table intro: This summary shows each assessment step, what’s measured, and the typical result so families understand the process.
This breakdown demystifies the assessment and shows how findings map directly to recommended services and interim supports.
Most in‑home assessments are brief, non‑invasive, and focused on turning checklist items into a care plan aligned with the senior’s goals and living situation. If your family’s checklist shows multiple red flags, scheduling a free in‑home care assessment can clarify options and connect you to services like personal care (bathing, dressing), companion care (social support), medication management, or skilled nursing for clinical needs. With the assessor’s report, families can compare options, test services on a trial basis, and set review dates as needs change.
How a Free In‑Home Care Assessment Tailors Support
A free in‑home care assessment identifies which daily tasks a senior can safely complete and which need assistance, then matches findings to specific service types and visit frequency. Evaluators consider ADLs, IADLs, medication adherence, and home risks to recommend targeted interventions — hourly companion visits, daily personal care, or periodic skilled nursing checks. The assessment report serves as a neutral reference families can use to divide responsibilities, explore benefits eligibility, and plan measurable trial services. This evidence‑based approach helps move the family from concern to a clear care plan while preserving the senior’s autonomy.
Common In‑Home Care Services and When They Help
In‑home care services include companion care for social support and light tasks, personal care for hands‑on ADL help, medication management for safe administration, respite care for temporary caregiver relief, and skilled nursing for medical needs. Each service meets a different set of needs: companion care boosts social engagement and assists with errands; personal care covers bathing and mobility help; skilled nursing addresses clinical monitoring and complex medication regimens. Assessment results guide selection of one or a combination of services and help set trial periods to evaluate fit and outcomes.
This comparison helps families match assessment findings to appropriate services and decide on trial durations.
How Caregivers and Families Can Manage Holiday Stress
Holiday caregiving adds emotional and logistical pressure, so realistic planning, scheduled breaks, and shared responsibilities are essential to protect caregiver health and preserve care quality. Self‑care practices and short‑term respite reduce burnout risk while ensuring the senior’s needs are met. Below are practical strategies and a table comparing common respite options, their typical duration, and caregiver benefits to help you choose sustainable relief during busy times.
Practical self‑care habits caregivers can adopt during the holidays:
Schedule regular breaks: Block short, predictable times to rest or run errands.
Delegate specific tasks: Assign concrete holiday roles to siblings and friends.
Set realistic expectations: Limit events and simplify plans to lower stress.
Use short‑term respite: Arrange daytime or overnight respite to recharge.
These tactics help preserve caregiver capacity and model a sustainable approach to long‑term responsibilities.
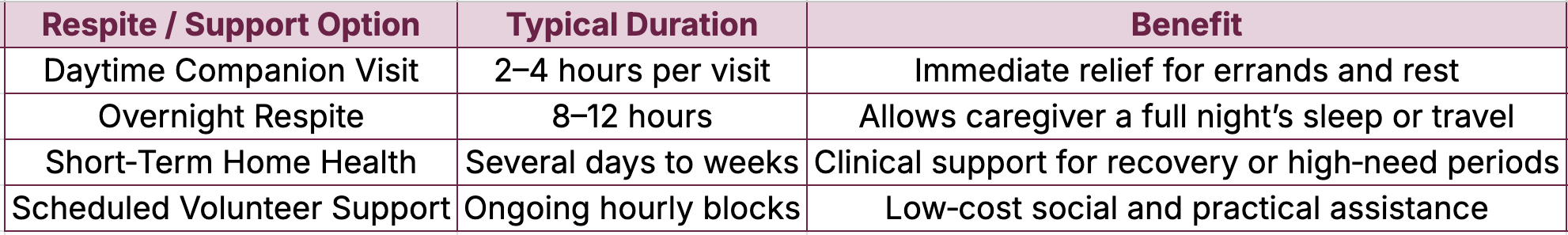
Respite options intro: The table below compares respite and support choices by typical duration and caregiver benefit to help select the right temporary relief.
This comparison shows how different respite options offer scalable relief so family caregivers can maintain well‑being and consistent care.
Practical Self‑Care Tips for Caregivers Over the Holidays
Start with realistic planning: limit the number of events, set clear boundaries, and schedule short restorative activities like brief walks or timed naps. Ask family members to commit to specific tasks — cooking, visits, or observation — so responsibilities don’t fall to one person. Use micro‑breaks (five minutes of deep breathing or a quick call to a supportive friend) to ease acute stress. When possible, arrange short‑term respite or companion visits during peak days to ensure both the senior and caregiver have coverage.
How Respite Care Provides Measurable Relief
Respite care temporarily replaces the primary caregiver, giving time for rest, travel, or focused attention on other responsibilities. Options range from a few hours of companion visits to overnight stays or several days of home health support for recovery. These services reduce burnout, lower stress‑related mistakes, and improve long‑term caregiving sustainability by creating predictable recovery windows. Families can arrange respite after a free in‑home care assessment to make sure services match the senior’s needs and the caregiver’s recovery plan.
Conclusion
Opening thoughtful conversations about in‑home care during the holidays can improve an older loved one’s safety and quality of life while strengthening family collaboration. By observing key signs, documenting facts, and using structured, empathetic conversations, families can move from concern to concrete, person‑centered plans. A professional in‑home care assessment is often the next best step to bring clarity and peace of mind. Discover how our services can help you navigate this important journey today.