Differences Between Home Care, Home Health, and Hospice: A Complete Guide to In-Home Senior Care Options
Many families face confusion when comparing home care, home health, and hospice because the services overlap in setting but differ sharply in goals, providers, and eligibility. This guide clarifies those differences, explains who benefits from each option, and offers practical scenarios and transition guidance so you can decide with confidence. You will learn clear definitions of non-medical home care, skilled home health care, and hospice care at home, plus a side-by-side comparison of goals, services, payment sources, and typical durations. The article also addresses common misconceptions about hospice, maps realistic patient scenarios to recommended care pathways, and outlines how transitions are coordinated by clinicians and care coordinators. Read on for detailed service lists, three comparison tables, decision-making checklists, and exact next steps to arrange personalized assessments and support for aging in place.
What Is Home Care? Understanding Non-Medical Home Care Services for Seniors
Home care refers to non-medical in-home support provided by caregivers to help people with daily living tasks, preserve independence, and reduce caregiver burden. These services focus on activities of daily living (ADLs) and instrumental ADLs (IADLs) rather than clinical treatment, and they are delivered by trained caregivers or companion aides. The primary benefit is maintaining a familiar routine and living environment while preventing unnecessary institutionalization, and care models range from hourly visits to 24-hour support. Understanding this non-clinical foundation helps families choose between companion-focused services and clinical home health options when medical needs change.
What Services Does Non-Medical Home Care Provide?
Non-medical home care typically includes assistance with bathing, dressing, meal preparation, medication reminders, light housekeeping, and transportation. Caregivers provide personal care assistance for ADLs such as toileting and feeding, and they support IADLs like grocery shopping and bill paying, which helps older adults remain safe at home. Companion care and social engagement are essential components that reduce isolation and support mental health, while respite care gives family caregivers scheduled relief. Knowing these typical services clarifies why non-medical home care is often the first step for seniors who need daily help but not skilled medical interventions.
The core services of non-medical home care focus on personal care and daily living tasks for safety and comfort.
Companion services address loneliness and support cognitive engagement.
Respite care provides temporary relief for family caregivers to prevent burnout.
These service categories form a practical foundation for aging in place and often precede or complement clinical services when medical needs increase.
Who Benefits Most from Home Care Services?
Home care is well suited for frail seniors, individuals with early-stage dementia needing supervision, and those recovering from minor functional declines who do not require skilled medical treatment. Family caregivers benefit when home care provides respite and predictable routine support, enabling them to maintain employment or caregiving balance. Individuals with mobility limitations or needing transportation to appointments also gain safety and continuity through non-medical help. Identifying these recipient profiles helps families match service intensity to functional needs and plan for potential escalation to home health or hospice if clinical indicators change.
How Does Home Care Support Independence and Quality of Life?
Non-medical home care supports independence by preserving daily routines, enabling safe self-care, and facilitating participation in community life, which improves overall quality of life. Personalized caregiver support reduces the risk of accidents at home, addresses nutritional needs through meal preparation, and promotes social connection through companionship, all of which contribute to mental well-being. Evidence and surveys consistently show most older adults prefer aging in place; targeted home care services make that preference feasible for many households. Appreciating these quality-of-life outcomes clarifies why home care is often the first line of support in a graduated care plan.
What Is Home Health Care? Skilled Medical Care and Rehabilitation at Home
Home health care is skilled, clinically oriented care delivered at home by licensed professionals under a physician's order to address medical necessity and support recovery or chronic disease management. This model requires a doctor's order and typically serves patients who are considered homebound or have limited ability to leave their home for treatment, with goals centered on rehabilitation, wound care, medication management, and preventing hospital readmission. Skilled home health services are time-limited and outcome-driven, focusing on measurable improvements like restored mobility, healed wounds, or stabilized chronic conditions. Recognizing the clinical threshold for home health helps families and clinicians coordinate referrals and set realistic recovery expectations.
What Skilled Services Are Included in Home Health Care?
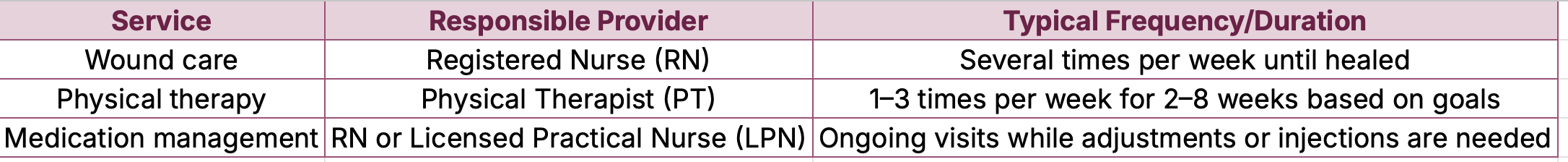
Skilled home health includes nursing services, physical therapy (PT), occupational therapy (OT), speech therapy (ST), wound care, and skilled medication management provided by licensed professionals. Registered nurses handle assessments, IV medications, and complex wound care; physical therapists focus on mobility and strength; occupational therapists support ADLs and adaptive strategies; and speech therapists address swallowing and communication deficits. These services are delivered according to a clinical plan of care designed to meet recovery milestones and reduce rehospitalization risk. Mapping services to licensed providers clarifies who does what during the rehabilitation process.
This table clarifies which licensed professionals deliver core home health services and sets expectations for typical visit cadence as part of an outcome-oriented plan.
Who Qualifies for Skilled Home Health Care?
Qualification for home health commonly requires a physician’s order, documented medical necessity, and homebound status or substantial difficulty leaving home, according to typical payer rules like Medicare guidance and clinical practice. "Homebound" generally means leaving home requires considerable and taxing effort or is medically contraindicated, and many referrals originate from hospital discharge planners or primary care providers. Payer rules vary, so care coordinators and home health agencies work with clinicians to document eligibility and create a plan of care aligned with coverage requirements. Understanding these referral pathways helps families navigate authorization and scheduling.
Medicare Home Care Certification: Eligibility Criteria and Physician's Role In order for patients to receive home care that is reimbursable by Medicare, the Health Care Financing Administration (HCFA) has ruled that a physician must certify the need for services at home and establish the plan of care.1This gate-keeping role may be appropriate for primary care physicians in many cases. However, nurses, therapists, or social workers may sometimes be better suited to determine home care eligibility because of the nature of the patient's condition or because, unlike physicians, they routinely make house calls.2Before 1989, coverage of home care services by Medicare was intended exclusively to provide short-term care after an acute illness or medical event. Since 1989, as a result of a lawsuit brought against the federal government by the National Association of Home Care on behalf of a patient (Duggan v Bowen), Medicare beneficiaries can receive in-home, long-term care so long as eligibility criteria continue to be met.1,3 Nonetheless, the eligibility criteria for home care remain stringent because the intent of the Medicare program is still generally to cover acute care rather than long-term care or preventive care. In addition, the clinical reality for many patients is that their chronic conditions exacerbate and improve over time, causing them to shift in and out of home care eligibility. These transitions further complicate the physician's role in determining patients' eligibility for home care services covered by Medicare. The purpose of this article is to discuss the role of the physician in authorizing and monitoring home care services given existing HCFA regulations. When physicians prescribe home care services for Medicare beneficiaries, they must certify that the patient (1) is homebound, (2) is in need of intermittent skilled nursing care, or physical, speech, or occupational the Eligibility for home care certification: what clinicians should know, 1998
How Does Home Health Care Aid Recovery and Prevent Hospitalization?
Skilled home health reduces readmissions by providing early post-discharge monitoring, medication reconciliation, wound surveillance, and timely therapy to restore function, which lowers complications and supports recovery. Rehabilitation milestones—such as walking a set distance or performing self-care tasks—are tracked and adjusted to reduce risk factors that lead to emergency care. Recent industry analyses and CMS guidance emphasize care coordination and transitional care as effective strategies to limit rehospitalization. By integrating skilled clinicians into the home environment, home health creates a bridge from hospital to independent living that improves outcomes and reduces system costs.
What Is Hospice Care? End-of-Life Comfort and Support at Home
Hospice care focuses on comfort, symptom control, and quality of life for patients with a limited prognosis, typically when curative treatment is no longer the goal and life expectancy is approximately six months if the illness follows its usual course. Hospice teams emphasize pain and symptom management, psychosocial and spiritual support, caregiver education, and bereavement services, and they coordinate care across home settings to honor patient preferences. The program is interdisciplinary—nurses, physicians, social workers, chaplains, and trained aides collaborate to relieve suffering and support families through end-of-life transitions. Understanding hospice as comfort-focused care clarifies how it differs fundamentally from curative-oriented home health.
What Services Are Provided by Hospice Care?
Hospice care provides pain and symptom management, nursing visits, aide services for ADLs, counseling for patients and families, medication and equipment related to comfort care, and bereavement support after a patient’s death. Clinical teams tailor interventions to maintain dignity and relieve distressing symptoms like pain, dyspnea, and agitation, while social workers and chaplains address emotional and spiritual needs. Volunteers often supplement care with companionship and practical assistance; hospice also arranges short-term respite to support family caregivers. These combined services create a holistic support system for both patient and family during the end-of-life phase.
Hospice offers clinical pain management to prioritize comfort over curative treatment.
Interdisciplinary teams provide psychosocial and spiritual support for patients and families.
Bereavement counseling is available to support family members after a patient dies.
These service categories show the breadth of hospice support beyond direct medical care, encompassing the whole family's needs.
When Should Families Consider Hospice Care?
Families should consider hospice when medical treatments no longer achieve meaningful improvement and the patient’s goals shift toward comfort, when a clinician estimates a prognosis of roughly six months if the disease follows its expected course, or when symptom burden outweighs potential benefit from aggressive interventions. Other indicators include frequent hospitalizations, progressive decline despite therapy, and patient or family preference for comfort-focused care at home. Initiating timely hospice enables better symptom control and family support, and it normalizes conversations about goals of care and advanced planning. Discussing prognosis and care preferences with the treating physician and care coordinator is the practical next step.
How Does Hospice Care Support Patients and Families?
Hospice uses an interdisciplinary approach—nurses manage symptoms; social workers coordinate resources; chaplains address spiritual concerns; and trained aides support ADLs—to ensure comprehensive comfort care and family-centered assistance. Bereavement counseling and caregiver education prepare families for end-of-life tasks and grieving, and hospice can provide short-term equipment and medication to maintain comfort at home. Coordination with primary clinicians and other providers ensures continuity of care, while volunteers and community resources supplement support. This team-based model reduces isolation, improves symptom control, and offers emotional and practical supports that extend beyond the patient's death.
What Are the Key Differences Between Home Care, Home Health, and Hospice?
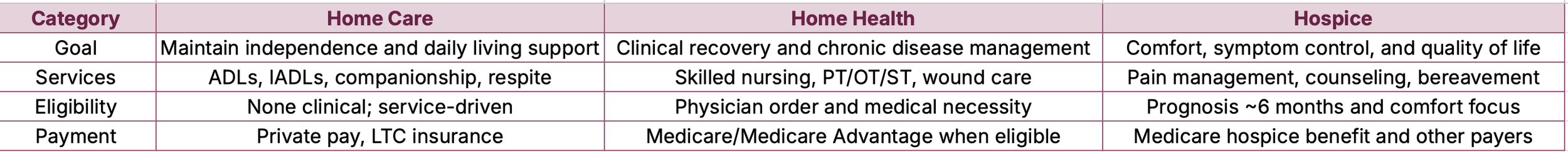
Understanding the core distinctions between these three in-home care types helps families choose services that match goals—maintaining independence, restoring function, or prioritizing comfort. Home care emphasizes non-medical ADL support and companionship to help seniors age in place; home health delivers skilled, outcome-driven clinical services under physician orders for rehabilitation or chronic disease management; hospice centers on palliative, comfort-focused care when life expectancy is limited. Payment sources, eligibility, typical providers, and expected duration vary significantly among the three, so a side-by-side view helps translate philosophical differences into practical decisions.
This comparison table provides a concise, scannable reference for goal, services, eligibility, duration, and payment differences across the three care types, helping families match needs to service models.
How Do Goals and Services Differ Among These Care Types?
The philosophical goals differ: home care promotes independence and daily comfort, home health pursues clinical recovery and stabilization, and hospice prioritizes comfort and dignity when cure is not the goal. Services map directly to those aims—home care focuses on ADLs and companionship, home health provides skilled therapies and medical nursing, and hospice delivers symptom management and family support. Recognizing these distinct aims clarifies which providers to engage and which outcomes to expect, helping families prioritize immediate needs versus long-term trajectories.
What Are the Eligibility and Duration Differences?
Eligibility varies: home care typically has no clinical eligibility and is arranged privately; home health usually requires a physician's order and documented medical necessity with possible homebound criteria; hospice generally requires clinician certification of prognosis and a shift away from curative intent. Duration for home care is open-ended based on need, home health is time-limited and goal-oriented, and hospice continues while eligibility criteria are met and can be extended if conditions change. These distinctions affect planning, funding, and the timing of care transitions.
How Do Payment and Funding Options Vary?
Payment sources differ across service types: home care is often private pay or covered by long-term care insurance; home health may be covered by Medicare, Medicare Advantage plans, or Medicaid when eligibility criteria are met; hospice has separate funding streams under Medicare and other payers that cover most hospice-related services. Recent trends show growth in Medicare Advantage influence on care coordination and prior authorization processes, impacting access and coverage nuances. Families should ask about payer rules and work with care coordinators to confirm authorization and out-of-pocket expectations.
Can You See a Side-by-Side Comparison Table of These Services?
Below is an accessible comparison table that highlights core rows—Goal, Services, Eligibility, Duration, Typical Providers, and Payment Sources—so readers can quickly scan differences and next steps. Use this table as a starting point to discuss options with clinicians and care coordinators.
This quick-reference table summarizes practical differences and supports conversations with providers and family decision-makers.
When Should You Choose Home Care, Home Health, or Hospice? Decision-Making Guide with Scenarios
Decision-making is clearer when you map real-world scenarios to likely care recommendations, identify transition triggers, and list the factors families should weigh such as prognosis, functional status, safety, and insurance coverage. Coordinated transitions typically involve the primary physician, case manager, and family caregiver, with documentation like physician orders or advance directives guiding changes. Below are concrete scenarios and recommended next steps to illustrate how needs align with service types and how to initiate transitions.
What Patient Scenarios Illustrate Appropriate Care Choices?
Below are common scenarios linking typical needs to a recommended care type and immediate next steps to take when you identify similar needs in your household.
When a scenario matches your situation, contact the treating clinician or care coordinator to request an assessment and appropriate referrals; documentation and physician orders are usually necessary for clinical services.
How Do Transitions Between Care Types Work?
Transitions are typically triggered by changes in medical status, goals of care, or after hospital discharge; they are coordinated by clinicians, discharge planners, or care coordinators who document new orders and adjust services. For example, a patient recovering from surgery may transition from home health to home care once rehab goals are met but daily assistance remains necessary. Effective transitions require clear communication among the physician, home health agency, home care provider, and family, along with transfer of medical records and a revised plan of care. Anticipating triggers and assigning responsibilities ahead of time smooths transitions and maintains continuity.
What Factors Should Families Consider in Choosing Care?
Families should weigh safety and functional needs, financial and insurance considerations, caregiver availability, prognosis and goals of care, and personal preferences regarding setting and routines. Safety assessments (home environment, fall risk) inform intensity of support needed, while insurance rules influence affordability and authorization timelines. Emotional readiness, cultural values, and family dynamics also shape whether to pursue hospice or continue restorative treatments. Prioritizing these factors and consulting clinicians and care coordinators helps match resources to the patient’s preferences and clinical reality.
What Are Common Misconceptions About Home Care, Home Health, and Hospice?
Misconceptions can delay appropriate care: many people mistakenly believe hospice means giving up hope, that home health is identical to home care, or that non-medical home care provides clinical treatments. Debunking myths clarifies choices and reduces stigma around hospice and palliative care. Below we present myth-versus-fact explanations and concise Q&A items to answer common PAA search queries and help families make informed decisions.
What Myths Surround Hospice Care and End-of-Life Services?
A common myth is that hospice hastens death or means abandoning the patient; in reality, hospice focuses on symptom control, dignity, and quality of life, and many patients receive meaningful comfort and family support. Another myth is that hospice ends all medical care—hospice shifts goals from cure to comfort but continues medical interventions that relieve suffering. Reassuring families and clinicians with clear explanations and compassionate language helps normalize hospice as a positive option when appropriate. Correcting these misconceptions encourages timely conversations about goals of care.
How Is Home Health Different from Home Care?
Home health requires a physician’s order and provides skilled services like nursing and therapy, while home care focuses on non-medical ADL assistance and companionship without clinical treatments. Home health is outcome-driven and often time-limited to meet rehabilitation goals, whereas home care can continue indefinitely based on need and funding. Understanding this distinction helps families avoid confusion when arranging services and ensures care matches clinical requirements or daily living needs. Clear examples—such as wound care delivered by a nurse versus bathing assistance provided by a caregiver—illustrate the practical differences.
What Are Frequently Asked Questions About In-Home Senior Care?
Below are concise, snippet-friendly Q&A pairs addressing common queries about qualifications, costs, and how to start in-home care, designed for clear, actionable answers.
How do I start home health services? Contact the treating physician to request a physician’s order and referral to a home health agency that will assess medical necessity and create a plan of care.
Does Medicare cover home health? Medicare may cover home health when eligibility criteria are met, including a physician order and medical necessity; coverage details vary by plan.
When is hospice appropriate? Hospice is appropriate when the patient’s goals shift to comfort and a clinician estimates a prognosis of roughly six months if the disease runs its normal course.
Can home care help with dementia supervision? Yes, non-medical home care can provide supervision, routines, and behavioral support to improve safety and quality of life for those with dementia.
What is a care coordinator? A care coordinator organizes services across providers, manages transitions, and helps families navigate eligibility, documentation, and payer rules.
How do I pay for home care long-term? Payment options include private pay, long-term care insurance, and sometimes community programs; planning ahead clarifies financial sustainability.
Why Is In-Home Senior Care Valuable? Benefits of Home Care, Home Health, and Hospice Services
In-home care delivers cross-cutting benefits: preserving independence, improving comfort, enabling personalized care plans, reducing hospital readmissions, and providing family caregiver support. Receiving care at home leverages familiar surroundings to reduce stress and confusion, while targeted clinical interventions at home support recovery and reduce complications that lead to rehospitalization. For families, in-home services offer practical relief—coordinated visits, schedule flexibility, and emotional reassurance—making caregiving more sustainable and enabling aging in place with dignity.
How Does In-Home Care Improve Quality of Life for Seniors?
In-home care improves quality of life by maintaining routines, enabling meaningful social contact, and tailoring support to personal preferences, which benefits both physical and mental health. Personalized care plans address nutrition, mobility, symptom management, and social engagement, reducing the risk of functional decline and institutional transitions. Recent research and industry reports emphasize aging-in-place preferences and show that coordinated in-home services can delay or prevent costly institutional care. These quality-of-life improvements make in-home options attractive for seniors seeking comfort, autonomy, and continuity.
What Are the Emotional and Practical Benefits for Families?
Families gain reduced caregiver burden, structured respite, and improved peace of mind when in-home care provides daily supervision and clinical coordination. Practical benefits include help with transportation, medication management, and communication with clinicians; emotional benefits include reassurance, improved family dynamics, and access to bereavement or counseling resources when relevant. Care coordinators and interdisciplinary teams also help families navigate payer rules and transitions, reducing administrative stress. These supports enable families to focus on relationships while professionals manage daily care tasks and clinical needs.
How Can You Schedule a Free Assessment or Contact for Services?
A simple, practical approach makes initiating care straightforward: prepare a brief summary of current needs, recent hospital discharges or physician recommendations, and any insurance questions; then contact the appropriate provider or care coordinator to request an assessment. During the free assessment, a clinician or care specialist reviews medical status, functional needs, home safety, and preferences, and then recommends a tailored plan with next steps and potential funding pathways. To provide comprehensive information about in-home senior care services and encourage potential clients to schedule a free assessment or contact them for services.
Step 1: Gather basic health and functional information and identify the primary decision-maker.
Step 2: Request a free assessment from a care coordinator or provider to review needs and create a plan.
This brief process clarifies expectations, expedites referrals for home health or hospice when clinically indicated, and helps families begin timely support for aging in place.
To provide comprehensive information about in-home senior care services and encourage potential clients to schedule a free assessment or contact them for services.